The best teaching comes from experienced mentors. We publish case studies from veteran functional medicine practitioners to help educate the community on how testing is related to root cause medicine. To order any of the tests from this case study, sign up for Rupa below.
[signup]
Chief Complaint: Fatigue, Weight Gain, Poor Sleep
Rebecca is a 44-year-old female who came into the clinic for her annual physical. She feels very fatigued and is dragging through the day. She has gained about 10 lbs in the last year and is having some new knee discomfort when she goes hiking. She has had a lot of stress at work over the last year and has traveled for at least one week every month. Her sleep has been disrupted with jet lag and early morning flights. She has not been exercising consistently and has been eating mostly on the go without much thought into what or when she is eating. She is not taking any supplements.
Overall, she feels less vibrant than she was a year ago and wants to “get back on track” and focus on her health.
Past Medical History
- She has had mild elevations in her cholesterol in the past with her LDL-C running between 110-130 on past lipid panels. Her triglycerides were less than 100 on prior labs.
- She has always had a normal fasting glucose and a Hgba1c less than 5.5.
This year, in addition to the usual labs we ordered for her annual, we added some advanced metabolic markers from Boston Heart to better understand her metabolic health.
Starting Lab Results
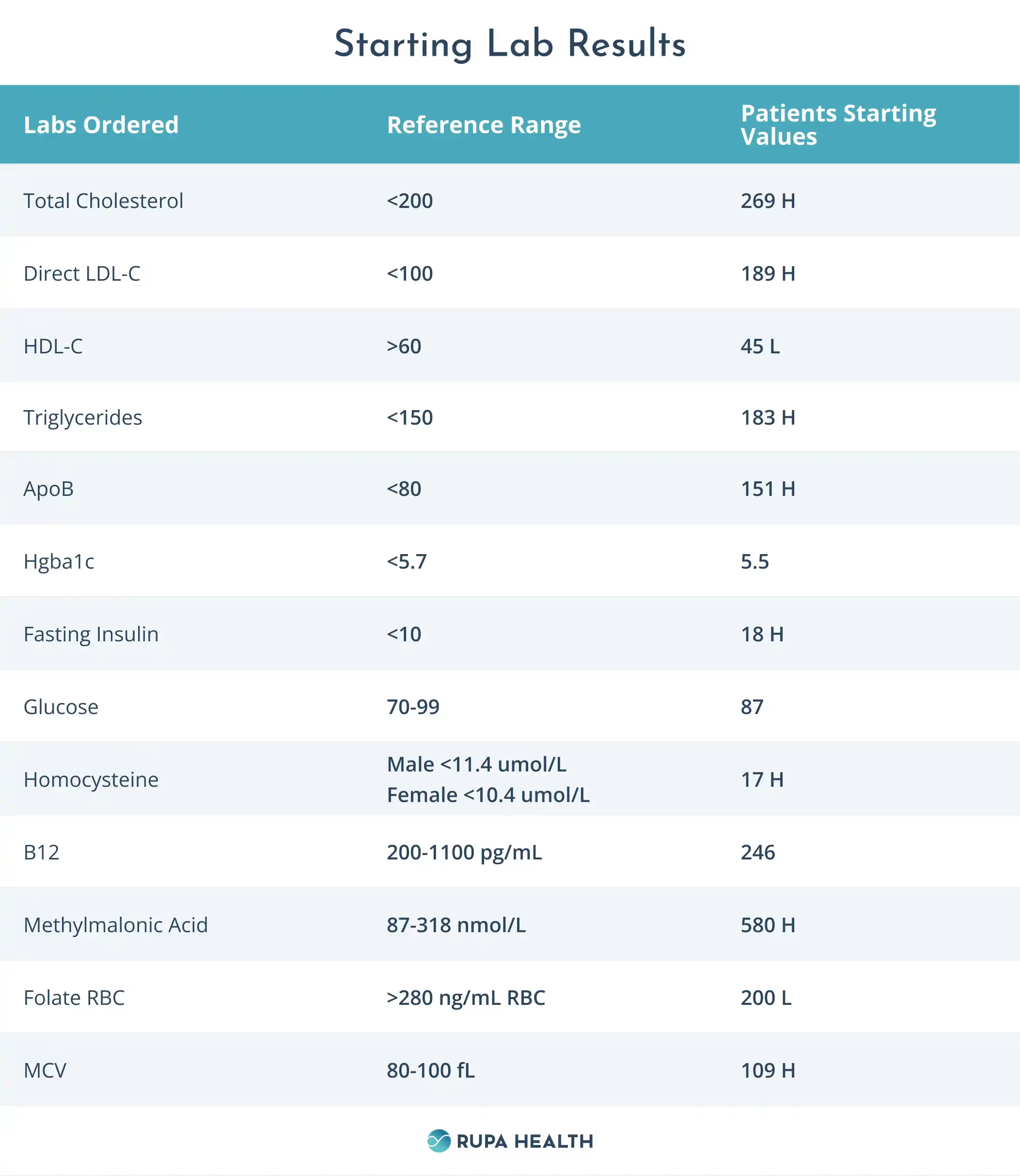
Lab Analysis
Indicators of Insulin Resistance
At face value, Rebecca’s Hgba1c is within the normal range. Hgba1c is a measure of glycosylation of red blood cells that gives us a proxy of average blood sugar levels over the lifetime of a red blood cell. If any health problems affect the size or quantity of red blood cells, it can alter the Hgba1c and render it a less effective proxy for average blood sugar. In Rebecca’s blood work, the increased size of the red blood cell (noted by the increased value of her MCV) may artificially lower her Hgba1c. Her fasting insulin level is quite elevated, suggesting significant insulin resistance, which is not being reflected in her Hgba1c.
Changes in LDL-C/ApoB and Triglycerides
Rebecca’s LDL-C/ApoB and Triglycerides are elevated and are above her usual baseline of triglycerides <100 and an LDL-C of around 100-130. Insulin resistance is often associated with an increase in triglycerides, a decrease in HDL, and an increase in the small dense sub-particles of LDL. These new changes in her lipid profile may indicate insulin resistance.
B Vitamin Levels and Homocysteine
Rebecca has multiple signs that may suggest B vitamin deficiencies, including an elevated MCV, elevated homocysteine, borderline low serum B12, and low RBC folate.
Interventions
Over the last year, Rebecca has experienced increased stress, disrupted sleep, and decreased exercise, which may contribute to weight gain and the onset of insulin resistance. The insulin resistance may be influencing her lipid profile, so the focus was on managing her insulin resistance first and then reassessing her lipids after improvements.
Rebecca’s Suggested Plan
- Consider using a continuous glucose monitor to observe post-meal glucose levels
- Start a B complex supplement
- Engage in exercise to the point of sweating for 30-45 minutes at least 3 times a week.
Continuous glucose monitors are small wearable devices that measure the glucose level in the interstitial fluid. They provide real-time feedback on how glucose levels respond to various foods and activities such as exercise and sleep. People are often surprised by how their bodies respond to foods they consider “healthy” and can adjust their diets based on real-time feedback. Many find this type of immediate feedback motivating, which can support behavioral change.
Note: Continuous glucose monitors are approved for use in insulin-dependent diabetics, so this will be an out-of-pocket expense for most patients and can be an expensive option to try.
Follow-up Labs 3 Months Later
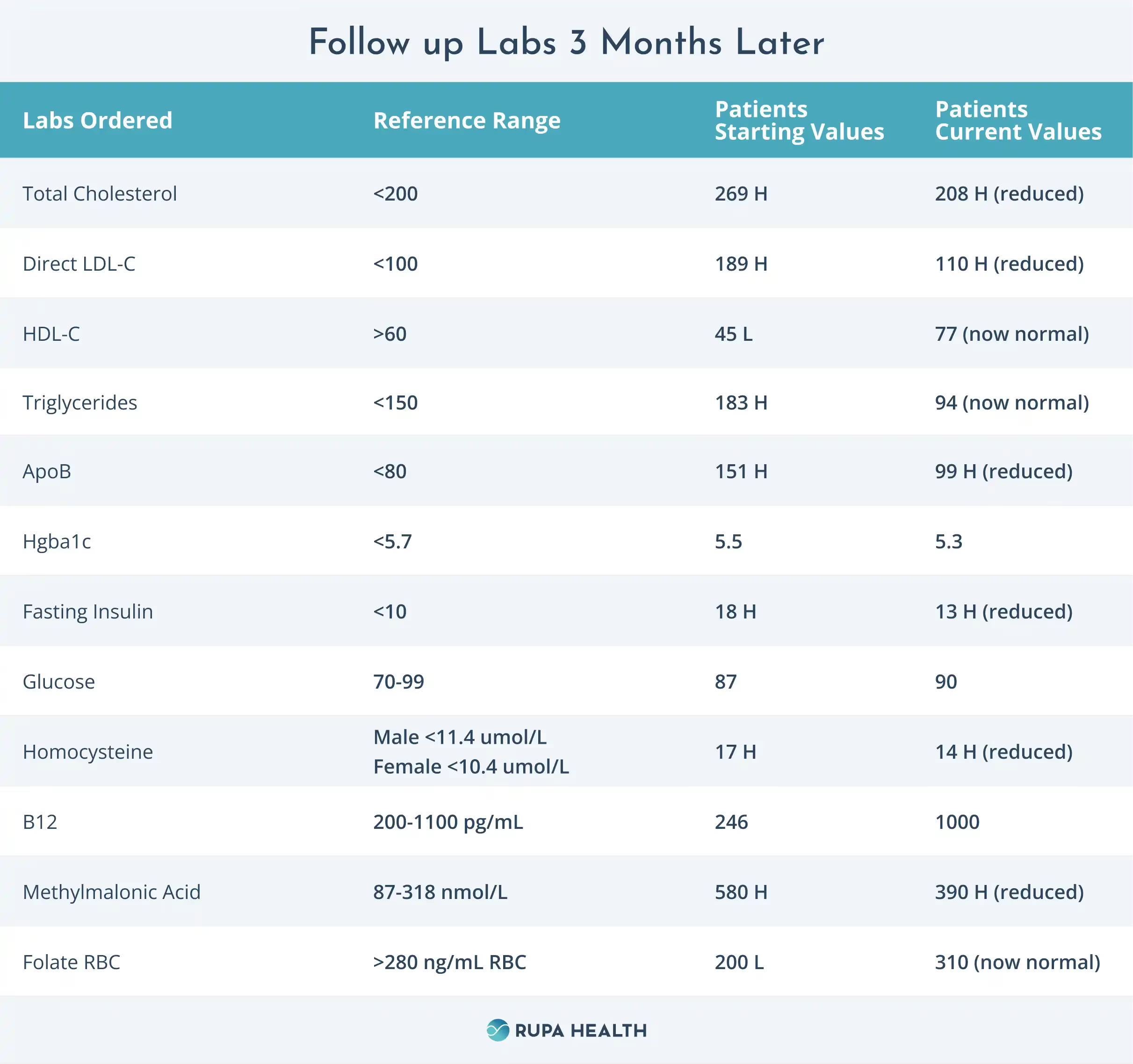
Outcomes
Rebecca found her continuous glucose monitor very helpful. She had previously been eating oatmeal for breakfast but noticed a significant glucose spike every time she tried it. She switched to eating a protein bar and stopped adding sugar to her coffee. Within two weeks, she noticed a reduction in her high morning glucose spike.
Over the one month she wore her monitor, she reduced her carbohydrate intake and started walking after larger meals like lunch or dinner. She was able to maintain these changes after she stopped wearing the monitor but thinks she would like to do it again in a few months for added motivation.
She is taking the B complex with no side effects.
She has started going for short jogs after lunch 3 times a week to get her exercise in and has been really enjoying that.
Overall, she feels a positive change in her energy and an improving sense of vitality. She didn’t expect it, but she has noticed an improvement in her sleep from these diet and exercise changes. She falls asleep easily and wakes up feeling more refreshed. She is also pleased that she has lost 5 lbs.
Reviewing her blood work, we can see that her fasting insulin and her Hgba1c have shown improvement. Her lipids have also trended back toward her baseline, and her B vitamin markers have also improved. She is encouraged to keep up these new diet and exercise habits with the plan to repeat her blood work again in 3-4 months.
Summary
Insulin resistance is often a factor in cellular problems that can lead to many physical symptoms as well as changes in other biomarkers.
Decreasing dietary carbohydrates, increasing exercise, and improving sleep can all help support metabolic health in the context of insulin resistance. Sustained motivation can be challenging when it comes to dietary and exercise interventions. Coaches, nutritionists, and wearable technologies such as continuous glucose monitors can all help support motivation and turn these changes into lifelong habits. Identifying insulin resistance early gives individuals the opportunity to make personal changes and support their overall health.












%201.svg)







