Acid Reflux is a common gastrointestinal issue, affecting about 20% of adults in western cultures. A typical approach to managing acid reflux involves the use of Proton Pump Inhibitors (PPIs).
Long-term use of these medications may be associated with side effects, including potential mineral deficiencies, kidney concerns, and bone health issues.
A Functional Medicine Approach to Acid Reflux includes specialty labs and lifestyle adjustments to address underlying factors.
Below is an example of such an approach.
[signup]
Chief Concerns: Acid Reflux, Bloating after eating, Fatigue, Gas
Taylor* was a 45-year-old female experiencing acid reflux that began 5-6 years ago. Initially, she found some relief with an omeprazole prescription from her primary care provider, but her medication no longer seemed effective. Over the past two years, she developed fatigue, gas, and bloating after meals.
She tried to reduce acidic foods (such as tomato sauce, hot sauce, citrus) in her diet, which seemed to help a little, but she was now experiencing reflux regardless of what she ate. The reflux was most noticeable at night when she was lying in bed, and she sometimes woke up with a burning sensation in her throat.
Taylor reported regular bowel movements every morning. Her fatigue seemed to last all day, no matter how much she slept, and she admitted to "pushing herself" a lot through the day, as she had a high-stress corporate position and was also a mom of 2.
Her recent blood work at the time was unremarkable, including a negative H. pylori test and endoscopy. While her general physician did not seem concerned, Taylor was worried because she "knew something wasn't right." She was frustrated that her reflux had only temporarily subsided, and the ongoing fatigue, gas, and bloating only added to her frustration.
Additional History
Taylor's lifestyle was an "on the go" lifestyle. She woke up early, went for a HIIT workout, came home to get her kids up and ready for school, then she and her husband both went to work at high-paced jobs.
Because her job was demanding, she admitted she often ate while working or on the go between meetings - the quicker, the better. She kept Justin's nut butter packets, almonds, and Rx bars at her desk to get her through the day when she didn't have time to eat an actual lunch.
When she got home from work, she immediately rushed into kids' extracurricular activities and household chores, with dinner often coming around 8 or 8:30 pm.
Since Taylor started experiencing more acid reflux at night, it took her a while to get comfortable and fall asleep. She was always up early to make sure she got a workout in before her day started, so her total hours of sleep were becoming reduced.
She had started drinking more coffee now to get through her day and was up to 4 cups per day, which she often took Tums with to help manage heartburn.
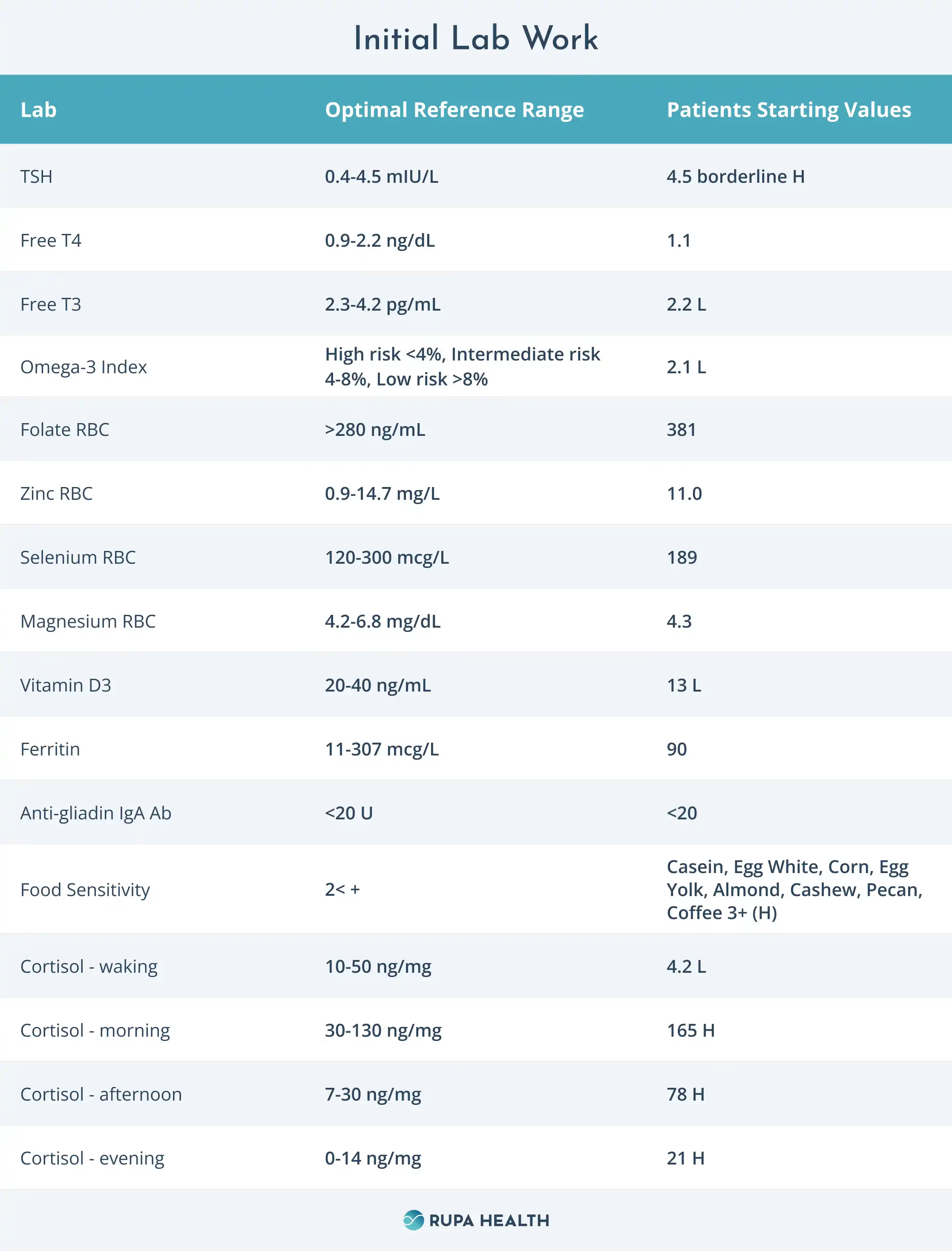
Initial Lab Work
GI Effects Comprehensive Stool Test Results
- Pancreatic elastase LOW
- Products of protein breakdown HIGH
- Beneficial SCFA's LOW
- Secondary bile acids LOW
- Fecal Fat HIGH
- Lactobacillus LOW
- Bifidobacterium LOW
- Zonulin Family Peptide HIGH
Other Relevant Lab Findings
From her primary care: Unremarkable endoscopy, negative H. pylori in endoscopy sample
Lab Analysis
Taylor's lab work suggests a few core issues that may contribute to her acid reflux and her more recent symptoms of fatigue, bloating, and gas.
Malabsorption and Impaired Digestion
Taylor's comprehensive stool analysis indicated impaired digestion and
malabsorption, as evidenced by higher amounts of fecal fat and products of protein breakdown, which we wouldn't expect to see if her digestive system was functioning optimally.
Additionally, low pancreatic elastase and bile acids suggest that her system may not be producing enough digestive enzymes to properly break down her food.
Dysbiosis
She also has low beneficial gut bacteria, such as Lactobacillus spp. and Bifidobacterium spp, which could indicate an imbalance in gut bacteria as an additional factor in her gastrointestinal symptoms.
Intestinal Permeability
Last, Taylor has elevated levels of the Zonulin family peptide, which has been associated with inflammation, imbalances in gut bacteria, and increased intestinal permeability, potentially increasing the risk of developing other health concerns.
Thyroid/Cortisol
Taylor's TSH is borderline high, while her free T3 is low. Taylor's high-stress, fast-paced lifestyle, lack of sleep, and early morning high-intensity workouts could be impacting her thyroid, contributing to her symptoms of fatigue.
Additionally, her 24-hour cortisol test showed elevated morning, afternoon, evening cortisol, and low waking cortisol, suggesting her stress response may not be ideal.
Not being able to shift from a sympathetic to a parasympathetic state could further contribute to digestive issues and fatigue.
Food Sensitivities
Several foods that Taylor is commonly eating - including almond butter, nuts, eggs (Rx bars), and coffee - all came back with high reactivity on an IgG food sensitivity test.
Her convenience foods may be contributing to her symptoms, even though she had been trying to "avoid" acidic foods per general acid reflux guidelines given to her by her primary care doctor.
Omega-3 & Vitamin D
All the above, paired with a low Omega-3 index and a low vitamin D level, suggests that Taylor is dealing with systemic inflammation impacting her health.
Functional Medicine Approach to Acid Reflux: Interventions
Nutrition
First and foremost, we worked on slowing down around meals, chewing food intentionally, and scheduling out some short breaks so that Taylor wasn't multi-tasking at work while she was eating.
- We set her up with a meal prep service that delivered "work lunches" 2x per week to her home so that she could take a balanced meal with her.
- We focused on cooked vegetables, broth-based soups, lean protein, and healthy fats like avocado, salmon, coconut oil, and olive oil.
- We adjusted her dinner time so that she wasn't eating dinner so close to bedtime, aiming for at least 2.5-3 hours between her last meal and going to sleep.
- Encouraged her to switch from coffee to matcha green tea to help her gut (coffee was a highly reactive food sensitivity) and her hormone function.
Supplements
We added in a few things to support her gut health, including:
- Apex-Energetics Repairvite SE: which contains zinc carnosine to help support the intestinal lining.
- Pure Encapsulations DGL Plus: 1 capsule before a meal. DGL helps coat the stomach, while aloe vera and slippery elm may support the gastric lining.
- Thorne L-Glutamine, 500mg per day: L-Glutamine has been shown to support gut health.
- Digestive enzyme with meals: To assist with breaking down fats, carbohydrates, and proteins.
- Magnesium glycinate, 250mg at night: Taylor's Magnesium RBC levels were bordering low. Magnesium is a vital nutrient for regulating many body processes. Magnesium glycinate in particular is good for sleep and stress reduction.
- Apex Energetics Adaptocrine: contains ashwagandha (may support T4-T3 conversion), as well as several other adaptogenic herbs to help with the body's stress response.
- Fish oil supplement, 2-4g per day: Her Omega 3 Index was low. Increasing her Omega 3's can help support a healthy inflammatory response.
- Vitamin D, 5000 IU per day: Her vitamin D levels were low.
Workouts
Workouts were modified: We planned out 2-3 days of more traditional strength training, with only one day of higher-intensity workouts, to help better regulate her hormones, stress, and inflammation. Taylor was encouraged to walk as much as she wanted to as well.
Sleep Hygiene
Last, I recommended that Taylor consider a wedge pillow at night if she was experiencing reflux while her therapeutic protocol started to take effect. She used it for about a week until her symptoms began to improve at night and now uses it just as needed.
4 Months Follow Up Labs

Follow Up Lab Analysis
When we re-ran labs and intake at four months, we saw several things trending in the right direction. By this point, Taylor was feeling significant improvement in her digestive symptoms and mainly only experienced reflux now if she ate too late at night or had too many of her "trigger foods" in a given meal.
She still felt low energy levels in the morning, but she was comfortable with her exercise routine and felt she could easily get through the day without the coffee.
She was falling asleep earlier since her reflux had improved as well.
Within a few weeks of removing the foods sensitivities, her gas and bloating had essentially disappeared.
She was consistent with her supplements, though she occasionally forgot her digestive enzymes if she was out to dinner or had a hectic day. She noted that she could feel a significant difference, mostly bloated if she didn't take them with meals.
We also added in a comprehensive probiotic supplement at this point to help support a healthy microbiome.
At this point, Taylor was interested in re-introducing some of the foods we had removed based on her labs, so I started her with a re-introduction tracker, adding in one food at a time and monitoring her energy levels and symptoms.
We checked in regularly over the next eight weeks. Taylor found that almonds caused a mild return of her symptoms of reflux and bloating, while corn resulted in bloating and gas, so she continued to leave those out of her diet.
We continued with her current supplement routine since she was doing so well, and at the 6-month mark, she decided she felt comfortable starting to remove the DGL gradually. She did not experience a return in her symptoms.
Last, we continued to focus on supporting healthy cortisol production through a combination of lifestyle, nutrition, and supplements: allowing time to unwind at night, a dark, quiet sleeping environment, not having caffeine first thing in the morning, ashwagandha, including enough protein and fat in her diet to keep blood sugar balanced.
Summary
This case highlights the need for a more integrative approach to managing acid reflux. For many, PPIs and other medications may provide temporary relief and might not address the underlying factors.
For Taylor, her acid reflux symptoms indicated underlying inadequate digestion and malabsorption and inflammation and imbalances in her gut. This placed additional stress on her body, only adding to the existing stress-related hormonal concerns and fatigue she was experiencing.
Functional medicine strategies can effectively help individuals with acid reflux and support a healthy gut.












%201.svg)







