Imagine feeling the urge to check the stove 20 times before leaving the house, believing there's only one “correct” way to organize your closet, and becoming upset when others don’t follow it. While both behaviors may seem obsessive, they reflect two very different mental health conditions.
Obsessive-Compulsive Disorder (OCD) and Obsessive-Compulsive Personality Disorder (OCPD) share features like perfectionism and rigidity, but they are distinct disorders with different causes, experiences, and treatment options.
This article explores the key differences and similarities between OCD and OCPD, explains how they are diagnosed, and reviews available treatment approaches.
[signup]
Defining OCD and OCPD
Before comparing OCD and OCPD, it’s important to understand what each disorder is and how it affects a person’s thoughts, feelings, and behaviors.
What Is Obsessive-Compulsive Disorder (OCD)?
Obsessive-Compulsive Disorder (OCD) is an anxiety-related mental health condition. It involves two main components:
- Obsessions: Persistent, unwanted thoughts, urges, or mental images that cause anxiety or distress. Common examples include fears of contamination, harm, or losing control.
- Compulsions: Repetitive actions or mental rituals (like handwashing, checking, or counting) performed in an attempt to reduce the anxiety caused by obsessions.
People with OCD are usually aware that their behaviors don’t make logical sense, but they feel powerless to stop them without significant distress.
What Is Obsessive-Compulsive Personality Disorder (OCPD)?
OCPD is a personality disorder defined by rigid thinking, perfectionism, and a strong need for control. Unlike OCD, it does not involve true obsessions or compulsions.
Instead, individuals with OCPD have long-standing personality traits such as:
- Preoccupation with rules, details, and organization
- Excessive devotion to work at the expense of leisure or relationships
- Reluctance to delegate tasks or accept others’ ideas
- Inflexibility and discomfort with change
These traits are consistent over time and are often seen as part of the person’s identity.
Key Differences Between OCD and OCPD
Though the names sound similar, the differences between OCD and OCPD are striking when you look at how each disorder affects thoughts, emotions, and daily life.
Nature of Thoughts and Behaviors
- In OCD, thoughts and behaviors are ego-dystonic, meaning the person knows they are unreasonable or unwanted and often feels distressed by them.
- In OCPD, traits are ego-syntonic, meaning the person sees their way of thinking or acting as correct or even admirable.
Insight and Awareness
- People with OCD usually have insight into their condition and seek help due to distress.
- People with OCPD often lack awareness that their behavior is problematic and may resist change, believing their methods are superior.
Impact on Daily Functioning
- OCD symptoms can significantly disrupt routines, take up hours of the day, and impair functioning.
- OCPD affects functioning in more subtle ways, often through strained relationships, micromanagement, or reduced productivity due to perfectionism.
Onset and Development
- OCD often begins in childhood or adolescence, sometimes triggered by stress or trauma.
- OCPD typically develops in late adolescence or early adulthood and reflects an enduring personality style rather than a cycle of symptoms.
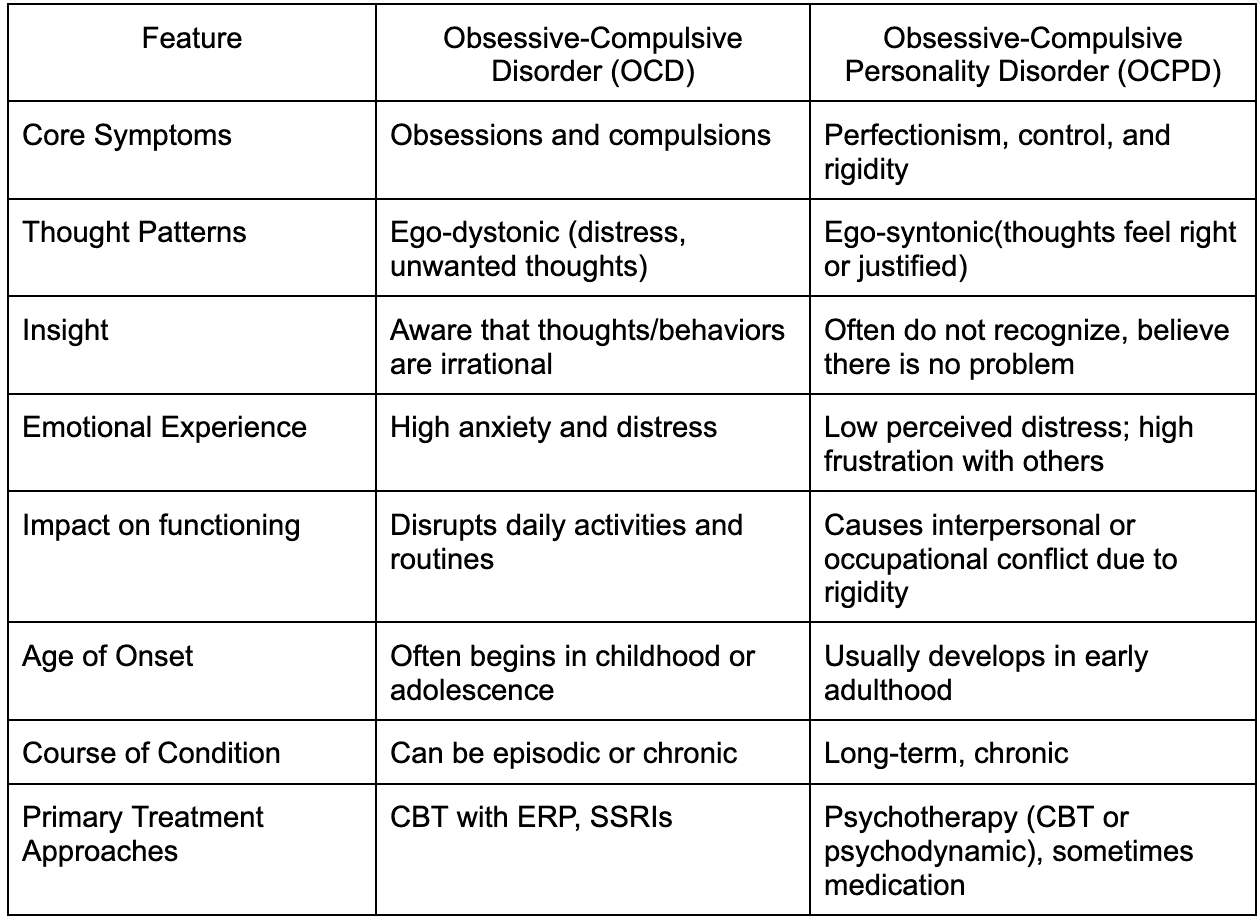
Table: Key Differences Between OCD and OCPD
Similarities and Potential Overlap
It’s easy to confuse OCD and OCPD because both may involve control, structure, or perfectionism. However, these traits stem from different motivations and internal experiences.
Common Themes in OCD and OCPD
- Perfectionism: Both may display a strong need to do things "just right."
- Rigidity: Difficulty adapting to change or accepting alternate ways of doing things.
- Attention to detail: A shared tendency to focus on order, cleanliness, or routine.
Despite these overlaps, the reasons behind the behavior are different. In OCD, actions are done to relieve anxiety. In OCPD, actions reflect a deep-seated belief that they are necessary or morally proper.
Comorbidity and Differential Diagnosis
- Some people may be diagnosed with both OCD and OCPD, though this is not common.
- Mental health providers must use careful clinical judgment to distinguish between these disorders, especially when symptoms overlap.
Causes and Risk Factors
Both OCD and OCPD can develop due to a combination of biological, psychological, and environmental influences. However, the specific mechanisms may differ.
Biological Factors
- OCD is associated with differences in brain structure and function, particularly in areas that regulate fear, impulse control, and repetitive behaviors.
- OCPD may have genetic influences, but biological evidence is less conclusive. It is often linked to temperament traits like conscientiousness and harm avoidance.
Environmental Influences
- Childhood adversity, including trauma, over-controlling parenting, or critical environments, can contribute to the development of both OCD and OCPD.
- Early experiences that reward perfectionism or self-control may reinforce OCPD personality traits over time.
Psychological Theories
- Cognitive-behavioral models of OCD suggest that people misinterpret intrusive thoughts as dangerous, leading to compulsive behavior aimed at reducing that perceived threat.
- In OCPD, developmental theories suggest personality traits form in response to childhood environments that value productivity, order, or rule-following above emotional flexibility.
Diagnosis and Assessment
Accurate diagnosis is essential to ensure individuals receive the appropriate care and treatment tailored to their unique condition. Because OCD and OCPD share some overlapping traits, such as rigidity and perfectionism, misdiagnosis is possible without a thorough evaluation.
Diagnostic Tools and Criteria
Mental health professionals rely on guidelines from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to make a diagnosis:
- OCD is classified as an anxiety disorder and is diagnosed when a person experiences persistent obsessions, compulsions, or both. These symptoms must cause significant distress, be time-consuming (typically more than one hour per day), and interfere with daily functioning.
- OCPD is classified as a personality disorder and involves a chronic pattern of preoccupation with order, perfectionism, and control. Symptoms often appear in early adulthood and are consistent over time, affecting relationships, work, and overall flexibility.
To gather this information, providers may use:
- Clinical interviews of patients, their family, and acquaintances
- Structured diagnostic tools (e.g., Yale-Brown Obsessive Compulsive Scale for OCD)
- Personality assessments or symptom checklists
- Self-report questionnaires and behavioral observations
Differential Diagnosis
Making a clear distinction between OCD and OCPD can be challenging, especially when a patient presents with symptoms like ritualistic behaviors or perfectionism.
- OCD must be distinguished from generalized anxiety disorder, specific phobias, and major depressive disorder, as these can also involve repetitive thoughts or behaviors.
- OCPD needs to be differentiated from other personality disorders, such as narcissistic personality disorder (which may include control-seeking behavior) or avoidant personality disorder (which can involve rigidity in social settings).
Understanding the underlying motivation and emotional response to behaviors, whether they are distressing or feel justified, can help guide diagnosis.
The Importance of Professional Evaluation
A licensed therapist, psychologist, or psychiatrist should conduct a comprehensive assessment, which may include a full psychiatric history, mental status exam, and symptom inventory.
This professional evaluation facilitates:
- Accurate diagnosis
- Appropriate treatment planning
- Identification of any co-occurring conditions (such as depression or ADHD)
The correct diagnosis is the first step toward getting meaningful support and improving quality of life.
Treatment Approaches
While both disorders can be treated effectively, the strategies often differ depending on the underlying causes and symptoms.
Evidence-Based Treatments for OCD
- Cognitive-Behavioral Therapy (CBT) with Exposure and Response Prevention (ERP) is typically the first-line treatment for OCD.
- Medications, such as selective serotonin reuptake inhibitors (SSRIs), can reduce the severity of obsessions and compulsions.
Therapeutic Strategies for OCPD
- Long-term psychotherapy, especially cognitive-behavioral or psychodynamic therapy, helps address rigid thinking and interpersonal issues.
- Behavioral strategies aim to improve flexibility, emotional expression, and relationship dynamics.
Integrative and Functional Medicine Perspectives
- Nutritional support, sleep hygiene, and stress management techniques can complement therapy.
- Functional medicine approaches may explore gut-brain health, inflammation, or hormonal imbalances contributing to mood and anxiety.
Living with OCD or OCPD
Managing a chronic condition involves more than clinical treatment—it requires emotional support, lifestyle adjustments, and personal resilience.
Coping Strategies and Self-Help Techniques
- Mindfulness, journaling, and deep breathing can reduce daily stress.
- Joining a support group helps individuals feel less alone and share coping tips.
Impact on Relationships and Work Life
- Honest communication with loved ones about the condition can reduce misunderstandings.
- Structured environments may benefit those with OCD or OCPD, but too much rigidity can limit personal growth or creativity.
Long-Term Management and Recovery
- Progress takes time—setting realistic goals and tracking small wins helps maintain motivation.
- Ongoing therapy and periodic reassessment can help prevent relapse and reinforce healthy coping skills.
[signup]
Key Takeaways
- Obsessive-Compulsive Disorder (OCD) is an anxiety disorder marked by intrusive thoughts (obsessions) and repetitive behaviors (compulsions) that cause significant distress and disrupt daily life.
- Obsessive-Compulsive Personality Disorder (OCPD) is a personality disorder characterized by rigid thinking, perfectionism, and a strong need for control, often perceived as appropriate or beneficial by the individual.
- OCD symptoms are ego-dystonic, meaning they are unwanted and cause distress, while OCPD traits are ego-syntonic, meaning they align with the person’s self-image and are not typically seen as problematic.
- OCD often starts in childhood or adolescence, while OCPD tends to emerge in early adulthood as part of a long-standing personality pattern.
- Although OCD and OCPD share traits like perfectionism and rigidity, they differ in motivation, insight, and emotional experience, making professional diagnosis essential.
- OCD is best treated with Cognitive-Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP), often alongside medication. At the same time, OCPD benefits from long-term psychotherapy focused on flexibility and interpersonal growth.
- A comprehensive evaluation by a licensed mental health professional is necessary to distinguish between the two and guide effective, personalized treatment.












%201.svg)







