Gastritis is a relatively common condition that affects the lining of the stomach. It can be caused by various factors, with the most common being an H. Pylori infection. Other causes can include different pathogens and non-microbial factors.
[signup]
CC: Chronic Gastritis, GERD, Generalized Anxiety Disorder, Fatigue
Anna was a 40-year-old female who experienced chronic symptoms such as burning in the chest and upper abdomen, bloating, gas, and long-term acid reflux. She had adjusted her diet over the years to help manage these symptoms. However, after losing her job and experiencing increased stress, her symptoms worsened. She had been dealing with these issues for 30 years, with multiple tests confirming gastroesophageal reflux without eosinophilic influence.
One year prior, she tested positive for H. Pylori and was treated with antibiotics, which left her feeling fatigued and nauseous.
Additional History
Anna recalled having gastrointestinal issues during her childhood, often resulting in hospital visits due to severe cramping, diarrhea, and vomiting. At age 12, she removed wheat, gluten, and dairy from her diet, which helped improve her symptoms.
She was tested multiple times for celiac disease, which was consistently ruled out. Anna also had a traumatic childhood and has been in therapy for the last ten years to help manage her PTSD and anxiety. She noticed some improvement in her bloating and abdominal pain with therapy, but not complete resolution.
Anna worked as a dental hygienist and maintained good dental care. Her diet was a modified paleo, allowing occasional potatoes and gluten-free grains while avoiding gluten and dairy.
She regularly consumed fermented foods, organic produce, and meat, avoided processed foods, and limited foods high in acidity like coffee, tomatoes, and citrus.
She had a sweet tooth and indulged in homemade treats on weekends, noticing increased symptoms afterward. She lived in a newly built home with her family for the last eight years, having moved from Poland at age 24.
Lab Work

Comprehensive Stool Test Results:
- Pancreatic Elastase Low
- Products of Protein Breakdown (Total*) High at 8.9 (1.8-9.9 micromol/g)
- Eosinophil Protein X (EPX) <detectable level (<=2.7 mcg/g)
- Fecal secretory IgA Normal at 444 mcg/mL (<=2,040 mcg/mL)
- Short-Chain Fatty Acids (SCFA) (Total*) Low at 13.5 (>=23.3 micromol/g)
- n-Butyrate Concentration Low at 2.1 (>=3.6 micromol/g)
- Acetate, n-Butyrate, Propionate % all within normal limits
Overall, the microbiota is healthy with no pathogenic or dysbiotic overgrowth. She also had high levels of beneficial bacteria: Akkermansia muciniphila, Collinsella aerofaciens, Ruminococcus spp, Lactobacillus spp., and Faecalibacterium prausnitzii.
Lab Analysis
Anna's lab work suggests several factors that may be contributing to her chronic gastritis and GERD.
- High morning salivary cortisol and DHEA suggest adrenal function changes with high morning cortisol output.
- Positive H. Pylori breath test
- Low pancreatic elastase and increased products of protein breakdown
The lab findings align with her symptoms; high stress and anxiety may contribute to elevated DHEA and cortisol levels. Studies show that high cortisol levels can be associated with decreased stomach acid, which may contribute to slow digestion and acid reflux symptoms. Low stomach acid can also lead to high protein in the stool and low pancreatic output due to a lack of pH signaling. Over time, low stomach acid may contribute to bacterial overgrowth and increased susceptibility to gastric issues.
Interventions
Nutrition
- Consider including foods that may help manage H. Pylori growth: fennel, lavender, chamomile, turmeric, peppermint, ginger.
- Include prebiotic foods to support microbiota growth: Cooked and cooled white rice/potatoes, sweet potatoes, oats, beans, legumes, whole grains, green bananas, potato starch, and green banana flour.
- Incorporate foods high in short-chain fatty acids (SCFA): organic ghee, onions, chicory, bananas, artichokes, asparagus, garlic, leeks, broccoli, pistachios.
- Stick to 3 meals daily and avoid snacking between meals to help maintain stable blood sugar levels.
H. Pylori Supplemental Support
- Biofilm Defense (Douglas Labs): 1 cap daily on an empty stomach for 60 days, then stop. Start with this for 2 weeks with GastroMend and DGL plus.
- GastroMend-HP (Designs for Health): 2 caps, three times a day, with meals
- DGL Plus (Pure Encapsulations): 2 caps with morning meal, 2 caps with evening meal
- Annatto Tocotrienols with Black Cumin Seed Oil (Designs for Health): 2 caps, twice daily, with any 2 meals
Support High Cortisol Output
- Adren-All (Ortho Molecular): 2 caps in the morning upon waking, 1 capsule around 2 pm.
- Daily meditation, yoga, or gentle walks outside for 45 minutes
- Maintain regular sleep/wake cycles and healthy sleep habits: 2 hours before bed, avoid food, screens, strong lights, and intense physical activity. Opt for a nighttime routine to wind down; Epsom salt baths 3x weekly are recommended. Daily morning exercise to raise the heart rate for 30 minutes.
Follow Up Labs 2 Months Later
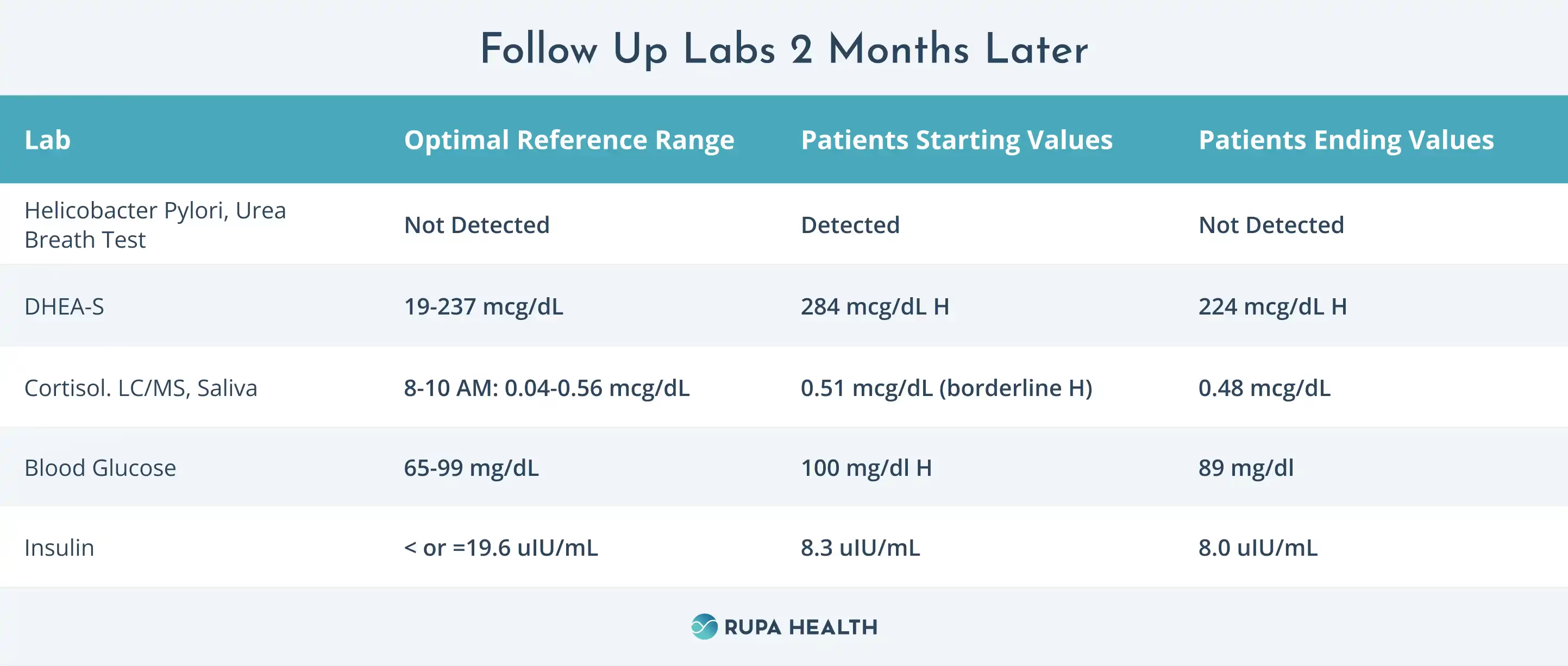
At our follow-up visit two months later, Anna reported feeling much better. Her gastritis symptoms had improved, and she only experienced occasional acid reflux when overeating or indulging in sweets.
Overall, her stress level was decreasing, she was sleeping better, and her energy levels had improved.
She successfully added lemon water at six weeks on the protocol without increasing symptoms, which she was pleased about as this was a morning staple for her.
She was advised to continue using the DGL and GastroMend supplements to help support her gastric lining while working on overall cortisol management and adrenal support through ongoing supplementation, therapy, and lifestyle changes. As she started a new job, her stress level increased, highlighting the need for continued adrenal support.
Summary
This case study illustrates the complex factors that can contribute to health issues, showing that it is rarely a single cause-and-effect process. Addressing multiple systems through lab testing, lifestyle changes, dietary support, and supplementation can work together to support long-term health and well-being.












%201.svg)







