Trying to get pregnant can be both exciting and overwhelming. Whether you're just coming off birth control or have been trying for a few months, there are many things you can do to support your body during this process. Fertility isn't just about timing—it's also about lifestyle, preparation, and understanding your body's signals. This comprehensive guide will help you learn how to improve your chances of conceiving naturally by optimizing your health for a safe and healthy pregnancy.
[signup]
Understand Your Cycle and Fertile Window
The menstrual cycle is more than just a few days of bleeding every month—it's often considered a woman's fifth vital sign and a window into her fertility.
Menstrual Cycle Basics
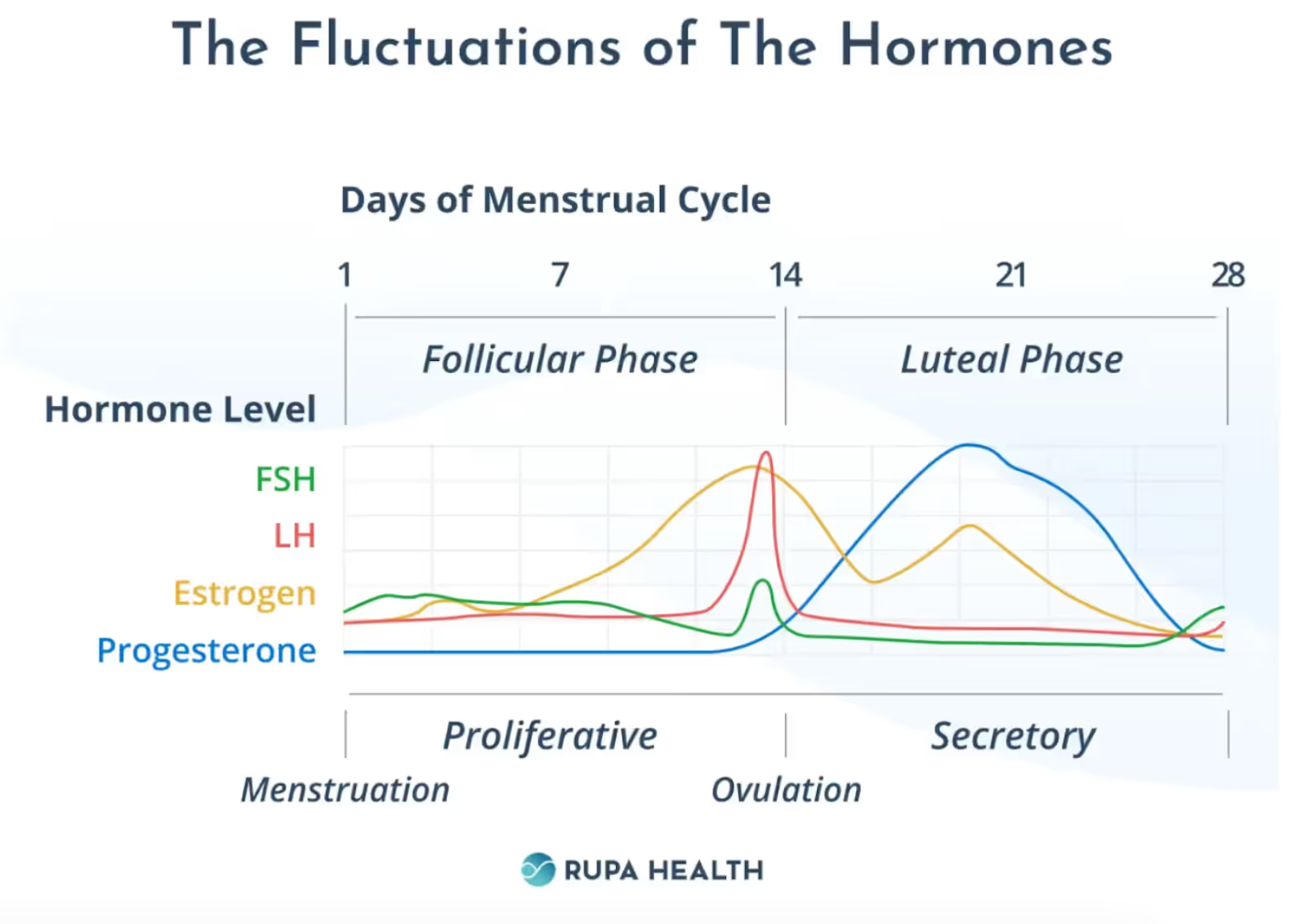
The menstrual cycle is a monthly process that a woman's body goes through to prepare for a potential pregnancy. It involves a series of monthly and cyclical hormonal changes that regulate the release of an egg, the thickening of the uterine lining, and the shedding of the lining if pregnancy does not occur.
A healthy menstrual cycle is typically around 28 days but can vary from person to person. It is divided into four main phases:
- Menstrual Phase: This is when bleeding occurs, marking the start of the cycle. It usually lasts 3-7 days and represents the shedding of the uterine lining from the previous cycle.
- Follicular Phase: This phase overlaps with the menstrual phase and lasts until ovulation. During this time, the pituitary gland secretes follicle-stimulating hormone (FSH) to stimulate the growth of ovarian follicles, which in turn produce estrogen to thicken the uterine lining.
- Ovulation: The follicular phase culminates in a luteinizing hormone (LH) surge caused by the rising estrogen levels during the first half of the menstrual cycle. This triggers the release of a mature egg from the ovary, typically around day 14 in a 28-day cycle.
- Luteal Phase: After ovulation, the body prepares for a possible pregnancy. The ruptured follicle turns into a structure called the corpus luteum, which secretes progesterone to maintain the uterine lining. If the egg is not fertilized, the corpus luteum breaks down, leading to a drop in progesterone and the start of the next menstrual cycle with the shedding of the uterine lining.
Identifying Your Fertile Window
The fertile window is typically a six-day period during every menstrual cycle when a woman is most likely to get pregnant. For most, this includes the five days before ovulation and the day of ovulation.
Fertility awareness methods (FAMs) are ways to track the menstrual cycle and pinpoint your fertile window. They include:
- Calendar Method: Track the length of your cycles. Mark the first day of your period (cycle day 1) and the first day of your next period. The total number of days in between the first day of each period is the cycle length. For women with regular menstrual cycles ranging from 26 to 32 days, the fertile window typically falls between days 8 and 19.
- Temperature Method: Measure your basal body temperature (BBT) in the morning, first thing in bed when you wake up. Body temperature rises by four-tenths of a degree after ovulation. Your fertile window is about two days before your BBT rises to three days after.
- Cervical Mucus Method: Check cervical mucus (vaginal discharge) daily to track changes in color and consistency. Cervical mucus that looks like egg whites signals you are in your fertile window.
Ovulation predictor kits (OPKs) are at-home urine tests that detect the LH surge to help identify the fertile window. Ovulation typically occurs 12 to 24 hours after the LH surge is detected in the urine. A Cochrane review found that urinary ovulation tests help increase the chance of live birth and clinical pregnancy for couples trying to conceive.
Tracking fertility is most effective when these methods are combined. This approach, known as the symptothermal method, increases accuracy in predicting ovulation and the fertile window.
Best Time to Have Sex to Conceive Fast
If you're trying to conceive, the best time to plan for intercourse is during the fertile window, or the six-day interval leading up to and ending on the day of ovulation. The Society for Reproductive Endocrinology and Infertility and the American Society for Reproductive Medicine recommend frequent intercourse (every 1-2 days) during this window to maximize pregnancy rates.
Peak fecundability (the period in a woman's menstrual cycle when she has the highest probability of conceiving) occurs within the two days before ovulation, with the highest likelihood of conception occurring the day before ovulation. The probability of clinical pregnancy increases from 3.2% on cycle day 8 to 9.4% on day 12, and decreases to less than 2% on cycle day 21.
Preconception Health and Lifestyle
In addition to tracking menstrual cycles, there are other things you can do to prepare for pregnancy and support fertility.
Health Check Before You Try
Preconception health screenings are an undervalued approach to supporting fertility. It’s wise to schedule a preconception checkup with your doctor, ideally 3-6 months before beginning to try to conceive. A thorough physical exam and comprehensive laboratory screening can help identify obstacles to a successful pregnancy.
Labs to ask your doctor about as part of a comprehensive prenatal exam include:
- Cardiometabolic Assessment – To screen for inflammatory and metabolic imbalances affecting egg quality, menstrual regularity, and pregnancy outcomes. Tests could include a CBC by Access Med Labs, the Comprehensive Thyroid Assessment by Genova Diagnostics, and the CardioMetabolic Profile by Doctor's Data.
- Reproductive Hormone Panel – To track hormones throughout a menstrual cycle to detect hormonal imbalances that may negatively affect ovulation, fertilization, or implantation. The DUTCH Cycle Mapping Plus by Precision Analytical (DUTCH) is one such example.
- Micronutrient Panel – To screen for nutrient deficiencies that may contribute to inflammation, menstrual irregularities, and poor pregnancy outcomes, helping to optimize health before and during pregnancy. The NutrEval FMV by Genova Diagnostics is an example.
- Vaginal Culture – To screen for vaginal infections, which are associated with infertility and preterm delivery. The Vaginosis Panel by Doctor’s Data tests for bacterial vaginosis and vaginal yeast overgrowth.
- Environmental Toxins – Exposure to environmental chemicals can cause hormonal imbalances and contribute to female infertility. Tests like the Environmental Pollutants Profile by US BioTek quantify toxic burden so that women can work to reduce exposures and support detoxification before becoming pregnant.
Diet and Supplements for Fertility
Nutrition clearly impacts reproductive health and fertility, as demonstrated by evidence that shows increased adherence to the Mediterranean diet is consistently associated with improved clinical pregnancy rates and live birth outcomes. Conversely, diets high in trans fatty acids, saturated fats, ultra-processed foods, and sugar-sweetened beverages are associated with poorer fertility outcomes.
Emphasize eating an anti-inflammatory, nutrient-dense diet rich in whole vegetables, fruits, nuts, whole grains, legumes, lean proteins, and olive oil. Eating a diverse array of foods ensures a broad intake of fertility-supportive nutrients, including calcium, iron, selenium, zinc, vitamins A, B9, B12, C, and E.
The United States Preventive Services Task Force (USPSTF) recommends that all women who are planning a pregnancy or could become pregnant take a daily supplement containing 400 to 800 μg (0.4 to 0.8 mg) of folic acid starting at least one month before conception.
In addition to folic acid, other micronutrients recommended during preconception and pregnancy include:
- Iron
- Vitamin D
- Calcium
- Iodine
- Omega-3 fatty acids
- Choline
Lifestyle Choices That Impact Fertility
Lifestyle interventions and modifications are generally cost-effective compared to conventional therapies. Adopting a healthy lifestyle before becoming pregnant positively influences fertility and reduces the risk of adverse pregnancy outcomes.
Weight Management
Being overweight or obese can contribute to hormonal imbalances, ovulatory dysfunction, and poorer reproductive outcomes. Weight loss, when indicated, has been shown to improve fertility outcomes.
The American Society for Reproductive Medicine recommends weight management programs focusing on preconception weight loss (specifically 10% reduction in body weight) to improve ovulatory function and pregnancy rates in obese women.
Substance Use
Heavy alcohol consumption, smoking, and excessive caffeine intake are all associated with negative impacts on fertility. It is advisable for individuals planning to conceive to limit alcohol and caffeine intake and to avoid smoking to optimize their chances of pregnancy.
Specifically:
- Limit alcohol intake to no more than one drink per day.
- Limit caffeine intake to no more than 200 mg daily (about 1-2 cups of coffee).
- Women and their partners who smoke should quit before they become pregnant.
Exercise
Sedentary behavior and physical inactivity are independent risk factors for infertility in both men and women.
Conversely, moderate-to-high levels of physical activity are associated with a reduced risk of infertility. Incorporating regular exercise into a preconception health plan can improve pregnancy and live birth rates, particularly in women with polycystic ovary syndrome (PCOS).
Stress Reduction
The hypothalamic-pituitary-adrenal (HPA) axis, activated by stress, inhibits the hypothalamic-pituitary-ovarian (HPO) axis, leading to menstrual irregularities. Relaxation interventions, such as yoga, progressive muscle relaxation, and mindfulness, have been shown to reduce maternal stress, anxiety, and depressive symptoms, which can improve reproductive outcomes.
Male Fertility Matters
So far, much of this article has focused on female fertility. However, don't let that fool you—male fertility is an equally important component to this equation. In fact, male factor infertility is responsible for up to 30% of infertility cases.
Supporting Sperm Health
Sperm quality and quantity in men have significantly declined in the last 40 years. Just as women can implement lifestyle, dietary, and supplemental strategies in their prenatal care to support menstrual and ovarian health, men can take similar steps to support sperm health.
Six key parameters influence sperm health:
- Semen volume
- Semen viscosity
- Sperm count
- Sperm vitality
- Sperm morphology
- Sperm motility
To optimize sperm health:
- Do not smoke or use drugs
- Avoid excessive alcohol consumption
- Reduce exposure to environmental chemicals and heavy metals
- Reduce genital heat exposure by avoiding prolonged sitting and tight-fitting clothing, limiting exposure to hot baths, and avoiding placement of electronic devices (e.g., cell phones and laptops) near the groin.
Specific nutritional supplements that may support sperm quality and quantity include:
- Antioxidants, such as selenium and vitamins C and E
- Omega-3 fatty acids, particularly docosahexaenoic acid (DHA)
- Coenzyme Q10 (CoQ10)
- Carnitine
- Zinc
When to Test Sperm Health
A semen analysis, along with a detailed male reproductive history, is recommended as part of an initial infertility assessment. Semen parameters are highly variable and can fluctuate significantly from one ejaculate to another. Therefore, at least two semen analyses, ideally obtained at least one month apart, are recommended, especially if the first analysis shows abnormal parameters. Multiple significant abnormalities in semen parameters increase the relative risk for male infertility.
Myths vs. Facts About Getting Pregnant Fast
Myth: You can't get pregnant right after your period.
Truth: Although it is less likely, getting pregnant right after your period is possible. For women with shorter menstrual cycles (e.g., 21 to 24-day cycles), ovulation can occur soon after the end of their period, increasing the likelihood of conception if intercourse occurs during or shortly after menstruation.
Myth: Morning sex improves the likelihood of conception.
Truth: Some evidence shows that sperm counts and quality might be slightly higher in the morning, particularly after 7-7.5 hours of a good night's sleep. However, there's no conclusive evidence that it significantly increases the likelihood of conception compared to other times of the day, and the key factor for conception remains timing intercourse within the fertile window.
Myth: You need to lie down after intercourse to improve the chances of conception.
Truth: Less than 1% of sperm stay in the female reproductive tract after intercourse. Anecdotally, some say lying down for at least 15 minutes after sex helps sperm get into contact with the cervix; however, the evidence doesn't support that this actually increases the likelihood of becoming pregnant.
Myth: Lubricants interfere with getting pregnant.
Truth: It is true that many commercial lubricants are associated with reductions in sperm motility and viability. To increase the odds of getting pregnant, the Society for Reproductive Endocrinology and Infertility and the American Society for Reproductive Medicine recommend using sperm-friendly hydroxyethylcellulose-based lubricants, like Pre-Seed®, which do not adversely affect sperm parameters.
Myth: I won't be able to get pregnant after age 35.
Truth: While the quality and quantity of a woman's eggs (oocytes) decline with age, particularly after 35, recent data shows that birth rates for older women have increased, and women can get pregnant and expand their families into their 30s and 40s.
When to Seek Medical Help
If you've been trying to get pregnant without success, it may be time to talk with a doctor.
General Timeline Based on Age
Conventional medical guidelines recommend fertility workups for women at different ages and stages of their fertility journeys:
- Women Under 35: Evaluation should begin after 12 months of unprotected sex, unless there are urgent medical concerns or physical findings.
- Women Over 35: Evaluation should begin after six months, due to age-related fertility decline.
- Women Over 40: Immediate evaluation is recommended because of the significant age-related decline in fertility.
For individuals with known medical conditions that may impact fertility (e.g., PCOS, endometriosis) or a history of fertility challenges, evaluation can begin earlier.
Diagnosing and Treating Fertility Issues
A fertility evaluation will begin with labs and imaging to rule out the most common causes of infertility in men and women, including:
- Ovulatory dysfunction due to thyroid dysfunction, hyperprolactinemia, PCOS, or hypothalamic amenorrhea
- Blockage of the fallopian tubes related to infections, endometriosis, or scar tissue
- Endometriosis
- Diminished ovarian reserve
- Uterine pathologies, such as polyps, fibroids, or scar tissue
- Male factors, such as varicocele, retrograde ejaculation, and hypogonadism
A doctor can help create a comprehensive and holistic treatment plan to address infertility. This can include simple modifications to lifestyle and supplement protocols to more advanced interventions like assisted reproductive technologies (ART).
Frequently Asked Questions (FAQs)
Can I get pregnant immediately after my period?
Yes, especially if you have a shorter menstrual cycle. Sperm can survive for several days in the female reproductive tract, and if ovulation occurs soon after your period, pregnancy is possible.
How can I tell when I'm ovulating?
Track your cycle, monitor cervical mucus, use OPKs, or chart basal body temperature for clues.
Does having sex every day increase my chances of pregnancy?
Not necessarily. It is recommended to have sex every 1-2 days during the fertile window to optimize the chances of pregnancy.
Should I be taking supplements even before I get pregnant?
Yes. It is recommended that a prenatal multivitamin be taken at least one month before trying to conceive.
[signup]
Key Takeaways
- Getting pregnant fast and naturally involves understanding your cycle, making healthy lifestyle choices, supporting your partner's fertility, and timing sex during the fertile window.
- While you can't control every factor, empowering yourself with knowledge and preparation can significantly boost your chances of a successful pregnancy.
- Want to learn more? Explore our related articles on tracking ovulation, the best foods for fertility, and early pregnancy signs.












%201.svg)






